Background
The Philadelphia chromosome t(9;22), a reciprocal translocation between chromosomes 9 and 22, results in the gene fusion BCR-ABL1, and occurs in 2-3% of childhood acute lymphoblastic leukemia (ALL). It is detected using cytogenetic and molecular techniques: karyotype, fluorescence in-situ hybridization (FISH) for t(9;22) and reverse transcription polymerase chain reaction (RT-PCR) for BCR-ABL1. Detection has implications for treatment, with the addition of tyrosine kinase inhibitors to chemotherapy regimens improving outcome.
Low level BCR-ABL1 transcripts have been reported in blood of healthy individuals. We have observed this finding in bone marrow in newly diagnosed ALL in the absence of the t(9;22) by karyotype or FISH. The significance of low level positivity at diagnosis has not been determined in the setting of childhood Philadelphia chromosome negative (Ph-) ALL. Here we report, for the first time, the molecular evolutionary characteristics of children and adolescents with low level BCR-ABL1 positivity found at diagnosis to relapse.
Methods
We reviewed 327 patients aged 0-17 years diagnosed with ALL or Acute Leukemia of Ambiguous lineage (ALAL) at The Children's Hospital at Westmead, Sydney, Australia from 1 January 2010 to 30 June 2020. Those positive for the BCR-ABL1 gene fusion by RT-PCR, and negative for t(9;22) by karyotype or FISH were included. Demographics, cytogenetics at diagnosis and relapse, and outcome data were extracted from the medical record.
Qualitative BCR-ABL1 analysis was performed using multiplex RT-PCR, followed by nested PCR, on RNA extracted from diagnostic bone marrow (sensitivity 5x10-6). If positive, quantitation was performed using real-time RT-PCR with results expressed as the ratio of BCR-ABL1 over ABL1 (sensitivity 1x10-5). Each PCR included positive and negative controls.
Results
Of 313 (96%) evaluable patients diagnosed with ALL or ALAL at our institution in the study period, 54 (17%) were positive by RT-PCR for BCR-ABL1 in diagnostic bone marrow. Seven patients were excluded as they had Ph+ ALL-specific treatment after the detection of t(9;22) by karyotype, FISH or other methods.
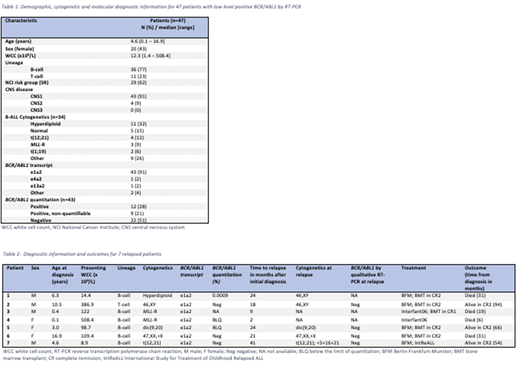
Forty-seven (15%) children with Ph- ALL had low level BCR-ABL1 detected by qualitative PCR. Demographic and cytogenetic characteristics for these patients are summarized in Table 1. All were diagnosed with ALL, the majority (77%) of precursor B-cell lineage including 2 with infant ALL. The e1a2 transcript was identified in 43 (91%) patients, with other transcript types as follows: e4a2 in 1 (2%), e13a2 in 1 (2%), and splicing variants in 2 (4%).
BCR-ABL1 quantitation was performed in 43 (91%) and was quantifiable only in 12 (28%) patients, with a median of 0.0008% (range 0.0003 - 0.095%).
Forty-five (96%) patients were treated with Berlin-Frankfurt-Munster ALL chemotherapy regimens. The two infant ALL patients were treated on the Interfant06 trial. One received a bone marrow transplant (BMT) in first remission then died after relapse; the other relapsed and died before BMT.
Seven (15%) of 47 relapsed, occurring at a median of 21 months (range 2 - 41 months) after diagnosis. Characteristics of these patients are presented in Table 2. Four patients were tested for BCR-ABL1 by RT-PCR in relapse marrow samples; all were negative. No patient with low level BCR-ABL1 positivity at initial diagnosis was diagnosed with Ph+ ALL at relapse.
There was no difference in 5-year relapse-free (80% vs 83%, P = .451) or overall survival (86% vs 91%, P = .368) between children with low level BCR-ABL1 positivity (n=47) and those without (n=259).
Conclusion
BCR-ABL1 low level positivity detected by RT-PCR in the bone marrow of children with newly diagnosed ALL is a relatively common finding, and did not adversely affect outcome for patients treated for Ph- ALL using a contemporary risk-adapted approach. Importantly, this finding did not influence the molecular evolutionary characteristics at the time of relapse in our patient group.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal